John Ioannidis has written about the fact that many of the results in the biomedical research literature have never been replicated. And when scientists do try to replicate prior results, they often get contradictory outcomes. Contradictory results are part of science, and they are a sign that new hypothesis need to be considered. This paper is a great example of that.
The paper was published by Caricilli et. al. in December, 2011 in PLOS Biology and is entitled "Gut Microbiota is a Key Modulator of Insulin Resistance in TLR 2 Knockout Mice." The team of Brazilian scientists was working with mice that had been genetically modified to knock out the gene for toll-like receptor 2 (TLR 2), a component of the innate immune system. They found that these mice were insulin resistant and went on to develop a phenotype reminiscent of obesity and type 2 diabetes. This is in contrast to previous studies that showed the opposite effect in TLR 2 knockout mice. Same experiment, opposite result.
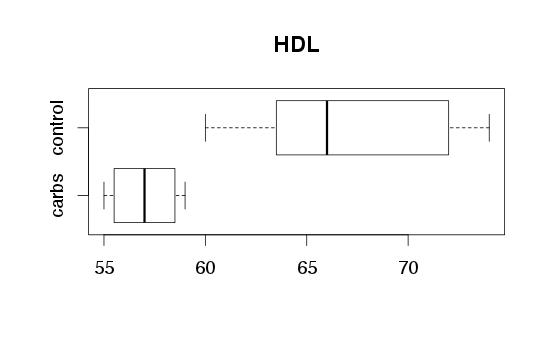
 |
| Three experiments from three labs. Conflicting results. |
The Brazilian team came up with a new hypothesis that might be able to explain all of the results. They showed that the genetic modification to the mouse's innate immune system resulted in changes to the composition of the mouse's gut flora. They believe that the gut flora, in turn, altered the mouse's insulin sensitivity. The effect depends on the flora present in the local environment in which the mouse is raised. This would be expected to vary from one lab to another. Therefore, a TLR2 mouse's insulin sensitivity may go up in some labs and down in others. The Brazilian team was careful to ensure that the mice they were using were raised not just in the same lab, but in the same room. Now that's some careful science.
The scientists characterized the gut flora of their control and TLR2 knockout mice (via sequencing 16S ribosomal RNA). They observed that firmicutes (a phylum of mostly gram-positive bacteria) are increased in their insulin resistant mice. When they transplanted this altered flora into healthy mice, they became insulin resistant too. When they used antibiotics which selectively kill off firmicutes in the TLR2 knockout mice, they went back to being insulin sensitive. Imagine that -- could we cure diabetes with antibiotics?
If you've read this far, you might be curious about your own microflora. Simply ship your feces to Metametrix and they'll analyze it by the same or a similar technique to that used in this paper. If you're insulin resistant, perhaps you have excess firmicutes and there may be strategies you can use to kick them to the curb. Of course mouse experiments do not necessarily translate to humans and healthy flora for a mouse will certainly differ from what is healthy in humans, but excess firmicutes have been found to be associated with obesity and diabetes in humans (in some but not all studies). Firmicutes have also been found to be reduced following gastric bypass surgery. A recent review paper by Tilg and Kaser (Gut Microbiome, Obesity, and Metabolic Disfunction) summarizes these findings. Of course, this information could turn out to be entirely useless -- perhaps it is not the categories of bacteria that matter, but specific strains, or the specific genes carried by (or expressed by) those strains. The interesting effects could depend not on what is there, but on the specific niches that particular strains have colonized (information that probably cannot be obtained from stool testing). We'll have to wait and see as this work is elaborated with new research, including the results of the Human Microbiome Project.
Is your Microbiome a Gland?
I mentioned above that the microbiome is in constant communication with your immune system and metabolic regulatory pathways. We saw from the Caricilli paper that changes in the microbiome can alter insulin sensitivity. One of the signaling molecules involved in this communication is lipopolysaccharide, or LPS. This is a component of the cell walls of gram negative bacteria. Your immune system is exquisitely sensitive to it. Concentrations measured in picograms per milliliter can cause measurable effects. This is a bit frightening when you realize that each of us is carrying around many grams (that's trillions of picograms) of LPS in our normal gut flora. Too much LPS and you die of sepsis, even if no live bacteria are present. Your immune system will kill you. For this reason, LPS has been referred to as bacterial endotoxin, though recent findings suggest it is much more than a mere toxin.
One very intriguing theory has been presented by John Marshall in a paper in Clinical Infectious Diseases (2005). He suggested that LPS should be thought of primarily not as a toxin, but as a hormone. It bears many similarities to our more familiar hormones. It exerts systemic effects by binding to specific receptors in multiple target tissues, triggering gene expression. It's effects are tightly regulated by a specific binding protein (creatively named "LPS binding protein") and multiple negative feedback loops. Typical of other hormones, it is harmful in excess, but beneficial in the right quantity and the right context. Of course it is quite odd for a hormone to be produced outside of your body, but in other respects it might fit the mold.
LPS typically spikes after meals, and has an acute systemic inflammatory effect. Going back to the mouse study, Caricilli et. al. found that their TLR2 knockout mice had higher serum LPS levels than the controls, and a greater increase in serum LPS following oral ingestion. The higher spike in LPS could be explained by the fact that the TLR2 knockout mice had lower levels of a tight junction protein that helps maintain gut barrier integrity. So it looks like an altered immune system resulted in an altered microbiome which changed intestinal barrier integrity which increased exposure to an exogenous hormone resulting in systemic inflammation, which caused metabolic dysfunction insulin resistance and obesity. Or, since the paper did not clearly establish cause and effect, any of the foregoing in any other causal permutation. Ok!
There is a lot more to say about LPS. What sorts of things cause it to increase, chronically or acutely? What regulates the body's response to it? And what about those curious negative feedback loops? More importantly, can we observe its effects through self-experimentation? Stay tuned for more.